Proton therapy is an advanced form of radiation treatment that is rapidly gaining attention for its precision and potential to spare healthy tissues. Unlike traditional X-ray (photon) therapy, proton therapy uses beams of accelerated protons that stop directly in tumors, minimizing collateral damage. Recent clinical trials and news from 2024–2025 show promising results: for example, a large phase III trial at MD Anderson found proton therapy achieved the same cure rates for head/neck cancer but significantly reduced malnutrition and feeding-tube dependence sciencedaily.com. Experts like Dr. Steven Frank emphasize that proton therapy offers “a curative, de-intensified option compared to traditional radiation therapy” sciencedaily.com. New compact proton systems are now under development, making this “life-saving treatment” more accessible to patients mevion.com, wusf.org.
What Is Proton Therapy and How Does It Work?
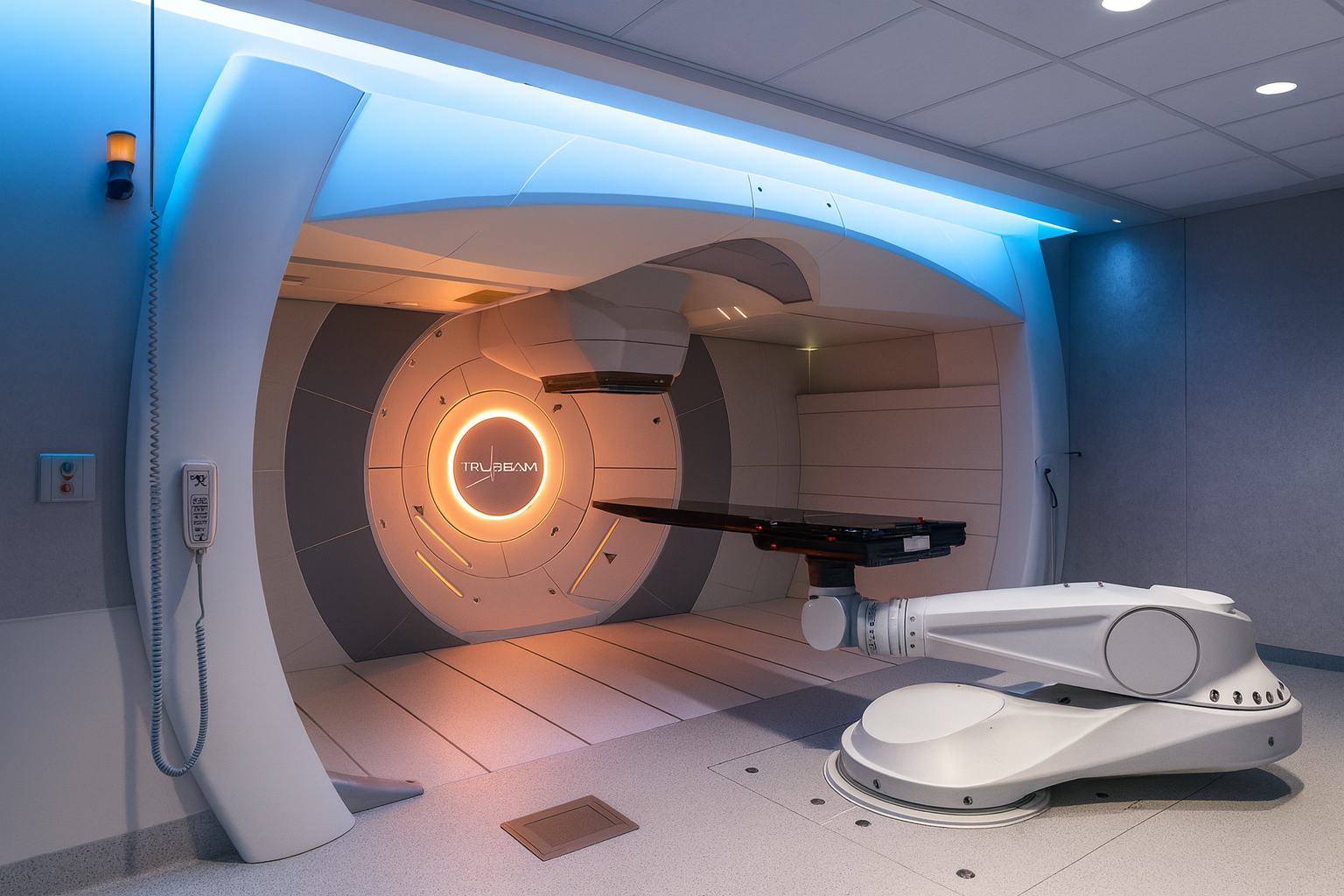
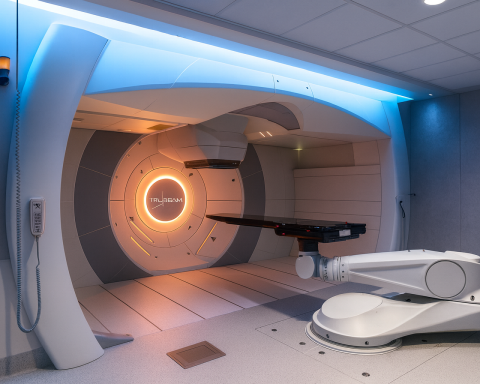
Proton therapy is radiation therapy using high-energy protons instead of X-rays. Special machines (cyclotrons or synchrotrons) accelerate protons to high speeds and direct them into the patient’s tumor. The key physics difference is the Bragg peak effect: protons travel through tissue and deposit a burst of energy right before they stop inside the tumor, with almost no exit radiation beyond it cancer.org, astro.org. This means proton beams can be tightly focused on the cancer. According to the American Cancer Society, this allows the radiation to “stop at the tumor and doesn’t go beyond it,” so less healthy tissue is damaged cancer.org. Mayo Clinic notes that by controlling where the protons deposit energy, doctors can often achieve fewer side effects than with photons mayoclinic.org, cancer.org. In practice, patients lie still while a proton gantry rotates around them, aiming the beam from multiple angles. Modern systems integrate imaging (CT/MRI) to precisely plan the proton paths.
| Feature | Conventional Photon (X-ray) Therapy | Proton Therapy |
|---|---|---|
| Beam Type | High-energy X-ray (photon) beams | Charged proton particles |
| Energy Deposition | Gradual dose through tissue; significant exit dose beyond tumor | Dose peaks at tumor (Bragg peak); no exit dose |
| Damage to Healthy Tissue | Significant normal tissue exposure along beam path astro.org | Minimal exit dose; sharper dose fall-off cancer.org |
| Precision / Control | Good (intensity-modulated RT), but beam passes through patient astro.org | Excellent (beam stops in tumor), sparing surroundings sciencedaily.com |
| Common Uses | Widely used for most cancers | Often used for tumors near critical structures |
| Side Effects | Higher risk of collateral damage (fatigue, skin changes, etc.) mayoclinic.org | Generally fewer, limited mostly to treated area mayoclinic.org |
| Equipment & Size | Linac machines (relatively compact) | Cyclotrons/synchrotrons (traditionally large, but new compact designs available wusf.org) |
| Cost | Lower (treatment course ~$13k for brain tumors in one study resource-allocation.biomedcentral.com) | Higher (about $1.4k more for brain tumors in Sweden resource-allocation.biomedcentral.com) |
| Availability | Very common (centers worldwide) | Limited (≈46 centers in US proton-therapy.org, ~100+ globally pubmed.ncbi.nlm.nih.gov) |
Benefits of Proton Therapy
- Greater Precision: By stopping protons at the tumor, clinicians minimize radiation to surrounding organs. This is especially important near the brain, spinal cord, or heart unmc.edu. Dr. Charles Enke explains, “the main benefit of proton therapy is the reduction of the radiation dose to the adjacent normal tissue. That says it in a nutshell” unmc.edu.
- Fewer Side Effects: Numerous reports note patients often experience less nausea, skin damage, and other side effects than with X-rays. For example, Mayo Clinic states studies suggest fewer side effects with proton therapy because doctors can better control beam delivery mayoclinic.org, cancer.org. In practice, treated patients still feel fatigue or localized skin changes, but systemic side effects are usually milder mayoclinic.org.
- Better Quality of Life: Trials show patients maintain higher quality of life during and after treatment. A 2024 ASTRO trial in prostate cancer found IMRT (photon) and proton therapy yielded equally excellent outcomes, but the potential is that protons could reduce late toxicities astro.org. Patient advocates highlight reduced risk of long-term complications (e.g. secondary cancers) as a key hope for protons protonbob.com.
- Pediatric Advantage: Children benefit greatly because protons spare developing organs. Experts note pediatric tumors are “among those who benefit the most,” since proton therapy spares healthy tissue in a growing child mayoclinic.org, unmc.edu. Proton therapy thus lowers the chance of growth issues or secondary cancers later in life.
Risks and Limitations
- Common Radiation Side Effects: Proton therapy is still radiation. Patients may experience fatigue, hair loss, or skin redness in the treated area mayoclinic.org. Side effects depend on the tumor site and dose. For example, head/neck treatment may cause sore throat or difficulty swallowing.
- Uncertain Long-Term Benefits: While protons reduce normal tissue dose, it’s not yet proven universally superior. Early studies show similar cure rates to photons in many cases sciencedaily.com, astro.org. Ongoing trials are clarifying where protons add value.
- Access and Cost: Proton therapy is significantly more expensive and less available. Specialized equipment and vaults raise costs and construction times. For patients, a Swedish study found a course of proton therapy for brain tumors cost ~$14,640 versus $13,308 for conventional RT resource-allocation.biomedcentral.com. In the US, Medicare generally covers proton therapy for approved indications, but patients face co-pays (about 20%) and deductibles medicalnewstoday.com. As ASTRO notes, “this increased precision also comes with significantly higher costs” and limited availability astro.org.
- Treatment Challenges: Proton beams are sensitive to tissue changes and patient movement. Ensuring accuracy requires careful planning. There is also variability in relative biological effectiveness (RBE) of protons, which can affect dosing decisions.
Which Cancers Are Treated with Proton Therapy?
Proton therapy is often chosen for tumors near critical organs or in children. Common indications include:
- Pediatric Cancers: Brain tumors, spinal tumors, and other childhood cancers (to limit late effects) mayoclinic.org, unmc.edu.
- Central Nervous System: Brain and skull-base tumors (e.g. chordoma, chondrosarcoma), where avoiding normal brain is key mayoclinic.org.
- Head and Neck Cancers: Tumors of the sinus, nasal cavity, oropharynx and other sites close to eyes, brainstem, or salivary glands mayoclinic.org, sciencedaily.com. Recent trials (e.g. for oropharyngeal cancer) highlight protons’ benefit here.
- Eye (Ocular Melanoma): Proton therapy can precisely treat eye tumors while sparing vision.
- Prostate Cancer: Especially low-to-intermediate risk prostate cancer. Large trials (PARTIQoL) show protons match IMRT in cancer control and quality-of-life astro.org.
- Spine and Bone Tumors: Vertebral or sacral tumors (e.g. sarcomas, chordomas) near spinal cord.
- Pediatric and Neurocognitive Conditions: Some non-cancer conditions (e.g. severe arteriovenous malformations in children) are studied.
- Re-irradiation Cases: When a tumor recurs in an area that already got radiation, protons can spare normal tissues that tolerated the first dose.
Numerous centers and trials are exploring proton therapy for other cancers (lung, liver, pancreatic, etc.), but insurance approval can be harder outside established indications. Mayo Clinic notes proton therapy “may also be used if the cancer remains or comes back after traditional X-ray radiation” mayoclinic.org. Always, an oncologist will consider all factors to recommend the optimal therapy.
Latest Clinical Research & News (2024–2025)
Recent studies have strengthened evidence for proton therapy in specific cancers:
- Head & Neck Cancer (2024): MD Anderson reported a Phase III trial comparing intensity-modulated proton therapy (IMPT) to IMRT in oropharyngeal cancer sciencedaily.com. Proton-treated patients had the same high cure rates but significantly less malnutrition and feeding-tube dependence. Dr. Steven Frank said this trial suggests protons could become “a new standard-of-care… a curative, de-intensified option” for these patients sciencedaily.com.
- Prostate Cancer (2024): The PARTIQoL trial (ASTRO 2024) randomized 450 men to proton therapy or IMRT astro.org. Results showed identical tumor control and quality-of-life with either method (5-year outcomes were both ~94% freedom from recurrence). Dr. Jason Efstathiou (MGH) emphasized both treatments were “very safe, effective…[with] excellent outcomes” astro.org. The report noted protons’ precise energy deposition but cautioned that equipment costs are much higher for proton therapy astro.org.
- Long-Term Survival (2025): At the 2025 National Proton Conference, Dr. Frank (MD Anderson) presented ten-year survival data for oropharyngeal cancer showing a significant overall survival benefit with proton therapy. Remarkably, the study also found protons to be more cost-effective than IMRT over the long term proton-therapy.org. A complementary retrospective study by Dr. Brian Baumann (Washington Univ.) also showed higher survival rates with protons in certain cancers proton-therapy.org. Experts commented that these findings could “fuel enthusiasm” and convince payors to expand coverage proton-therapy.org.
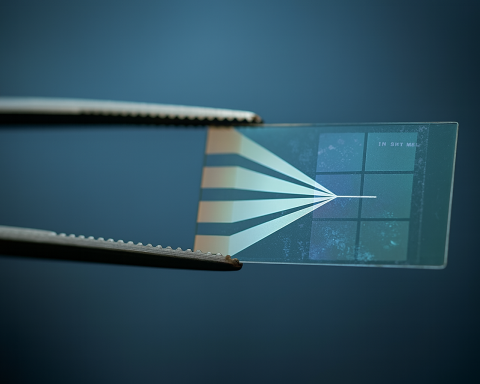
- Technology Advances (2024–25): Major manufacturers are developing compact proton systems. In January 2025, Mevion announced delivery of its first S250-FIT system to Stanford – designed to fit into a standard LINAC vault mevion.com. Stanford’s cancer center leadership said this will “enable us to expand access to proton therapy” without building huge new facilities mevion.com. Similarly, Nebraska Medicine broke ground on a new proton center (using an upright-treatment Mevion system) set to open in late 2025 unmc.eduwusf.org. These “small-footprint” units (Mevion’s, ProTom’s Radiance 330-C, etc.) can often be installed in existing clinics, drastically lowering construction cost and space.
- Patient Experience: Conferences have also focused on patient outcomes and equity. At NPC 2025, the American Cancer Society’s Dr. Arif Kamal urged integrating patient support and fair access into proton therapy programs proton-therapy.org. Media reports highlight patient stories, such as prostate cancer survivors finding “new hope” with protons. A Tampa news feature quoted board member/patient Don Ingram calling proton therapy “a lifesaving treatment” now locally available with the new BayCare center wusf.org.
Overall, the research community reports growing momentum: proton therapy is moving from niche to mainstream for select cancers, backed by hundreds of published studies and recent high-profile trial results proton-therapy.org.
Availability, Access, Cost and Insurance
Proton therapy remains far less available than X-ray therapy. Worldwide, 100+ centers operate pubmed.ncbi.nlm.nih.gov (mostly in the US, Japan, Europe), with dozens more planned. In the US there are about 46 centers as of 2025 proton-therapy.org. Access is uneven: NAPT notes over 70% of Americans live more than 100 miles from a proton center proton-therapy.org. Building large proton facilities has been a barrier – many required 50,000+ sq. ft. for their cyclotrons wusf.org. The new compact systems (which fit in ~2,000 sq. ft. or even existing vaults mevion.comwusf.org) are poised to spread proton therapy to community hospitals.
Cost: Building a center costs tens of millions; for example, BayCare’s new compact system is a $33M project wusf.org. For patients, a full course of proton therapy can run into tens or hundreds of thousands of dollars. A Swedish cost-effectiveness study (2024) found proton treatment for brain tumors cost about $14,640 vs. $13,300 for photon therapy resource-allocation.biomedcentral.com. In the US, Medicare generally covers proton therapy for approved indications (e.g. pediatric, brain/spine, eye cancers) medicalnewstoday.com, mayoclinic.org. Patients usually pay the standard coinsurance (around 20% of the Medicare-approved rate after deductible) medicalnewstoday.com. Commercial insurers may require prior authorization or consider protons investigational for some cancers mayoclinic.org. Mayo Clinic advises patients and families to work closely with insurers; “coverage varies by insurance company and disease type” mayoclinic.org.
Despite cost concerns, studies like the 2025 MD Anderson data argue that better long-term outcomes (e.g. fewer complications) could make protons cost-effective over a patient’s lifetime proton-therapy.org. For now, patients should consult financial counselors and insurance resources when considering proton therapy.
Expert Perspectives
- Dr. Charles Enke (UNMC Radiation Oncology): “The main benefit of proton therapy is the reduction of the radiation dose to the adjacent normal tissue… With pediatric patients… we also have to make certain they are not experiencing side effects of cancer treatment in 15-20 years” unmc.edu.
- Dr. Steven Frank (MD Anderson): Discussing head/neck trial results, Frank said proton therapy represents “a curative, de-intensified option compared to traditional radiation therapy” sciencedaily.com.
- Dr. Jason Efstathiou (MGH, ASTRO abstract): “We tested two… forms of radiation for a very common cancer, and we demonstrated that both are very safe, effective treatments that give patients excellent outcomes” astro.org.
- Sridhar Seshadri (Stanford Cancer Center): Commenting on the new compact system, he said: “This innovation reflects our commitment… The ability to integrate this system into an existing LINAC vault will enable us to expand access to proton therapy” mevion.com.
- Dr. Tina Yu (Mevion CEO): “This achievement underscores Mevion’s commitment to advancing proton therapy accessibility by developing systems that seamlessly integrate into existing radiation oncology workflows” mevion.com.
- Don Ingram (BayCare Board Member & Cancer Survivor): “This is a lifesaving treatment that can now be available to everybody here locally when it was not before” wusf.org.
- Dr. Samir Akach (BayCare CMO): “This is the most technically advanced cancer treatment. Just what all patients deserve” wusf.org.
These quotes, from leading physicians and advocates, highlight the growing excitement around proton therapy’s potential to improve patient care.
Recent News Highlights
- New Centers Opening: In September 2024 Florida’s BayCare health system broke ground on a compact proton center in Tampa (treating patients by late 2025) wusf.org. Nebraska Medicine announced in 2025 it would install a Mevion S250-FIT system in Omaha, the first in the region unmc.edu. Dozens of other centers (Penn Presbyterian, Moffitt, Tampa General, etc.) are under construction.
- Compact Technology: Mevion delivered its first S250-FIT “LINAC-compatible” system to Stanford in 2025 mevion.com. Other vendors (IBA, ProTom, etc.) are also marketing smaller, single-room systems. This trend is widely covered in medical news as a breakthrough for cost and access.
- Clinical Trials: The ongoing PARTIQoL prostate trial (published 2024) showed equivalence of protons and IMRT astro.org. The multi-institutional RADCOMP trial (for breast cancer) and others are ongoing. In pediatric oncology, initiatives like the NCI-funded Proton vs Photon cohort study (started 2023) aim to quantify long-term benefits stjude.org.
- Guideline Discussions: Centers like MD Anderson and Penn Medicine are reviewing recent evidence to update referral guidelines. Several institutions (MD Anderson, MGH, Texas Center, etc.) have published commentary on when to use protons.
- Access and Advocacy: Patient advocacy groups and professional societies have been vocal about insurance barriers. In 2024, ASTRO launched a toolkit to help patients appeal proton denials. The NAPT and other organizations are lobbying for broader Medicare coverage after the new trial data proton-therapy.org, wusf.org.
Overall, the last two years have seen proton therapy transition from a niche option to a serious contender for many cancer types, backed by rigorous trials and next-generation technology. As clinical evidence accumulates, many experts predict more widespread adoption in the coming years.
Sources: Authoritative overviews from Mayo Clinic and the American Cancer Society mayoclinic.org, cancer.org explain the basics and candidate cancers. Published studies and press releases (MD Anderson, ASTRO) provide clinical trial results sciencedaily.com, astro.org. News reports and hospital press releases supply recent developments and quotes mevion.com, unmc.eduwusf.org. All information is drawn from peer-reviewed studies, medical centers, and specialty news coverage as cited.