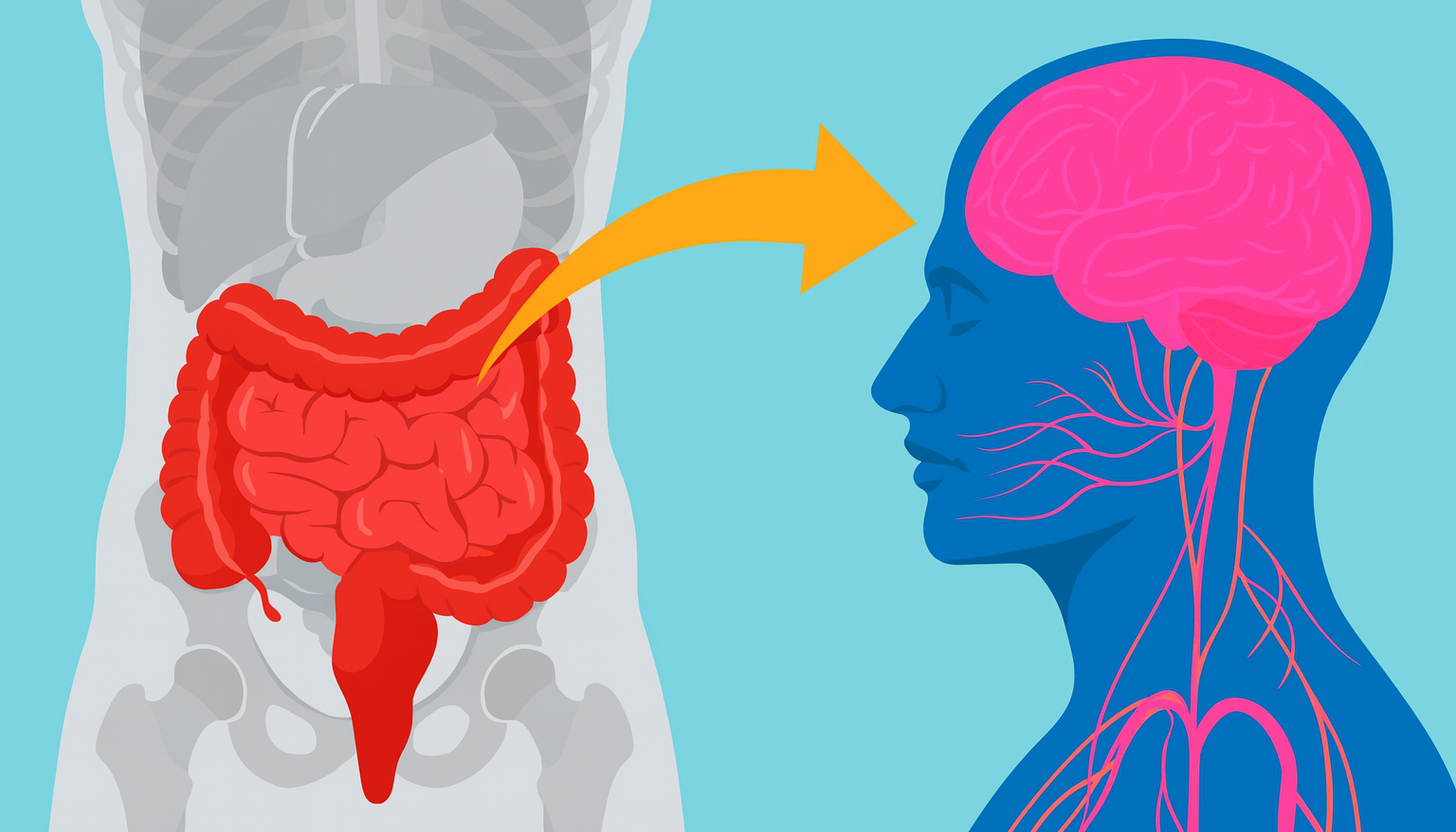
- The gut-brain axis is a two-way communication network linking gut microbes to the brain. Gut bacteria produce hormones, neurotransmitters and immune signals that travel to the brain (via the vagus nerve and bloodstream) nature.com, pmc.ncbi.nlm.nih.gov.
- Mental health: An imbalanced gut microbiome (dysbiosis) is linked to depression and anxiety. Depressed patients show distinct gut bacteria and metabolite profiles nature.com, and reviews note gut inflammation and dysbiosis correlate with anxiety/depression pmc.ncbi.nlm.nih.gov, health.harvard.edu.
- Cognition: Studies connect gut microbes to intelligence and memory. In young adults, a Ruminococcaceae-dominated gut community predicted higher fluid-IQ scores gutpathogens.biomedcentral.com. In schoolchildren, higher IQ was tied to greater gut microbial diversity and certain bacteria (Prevotella, Dialister, etc.) frontiersin.org. A 2020 review found most microbiome-intervention trials (probiotics, diet) improved memory, attention and learning pubmed.ncbi.nlm.nih.gov.
- Animal models: Experiments in mice show dramatic effects. Germ-free mice (with no gut bacteria) have abnormal brain development and overactive stress responses brainfacts.org. Transferring “depressed” human gut samples to rodents induced depressive and anxiety-like behaviors brainfacts.org, while transplanting microbiota from stress-resilient mice helped other mice recover from stress-induced depression and cognitive decline pubmed.ncbi.nlm.nih.gov.
- Interventions: Diet and probiotics can reshape the microbiome. High-fiber/plant-based diets support a healthy gut barrieri sappscience.org, whereas a Western low-fiber diet can impair it. Some clinical trials show probiotic supplements or prebiotics reduce anxiety/depression symptoms pmc.ncbi.nlm.nih.gov and even improve cognitive function pubmed.ncbi.nlm.nih.gov.
- Expert views: Leading scientists call the gut our “second brain.” Prof. Ted Dinan notes: “We all have a second brain… hundreds of millions of neurons [in the gut]… Its main job is transmitting information from the microbiota to the brain” gutmicrobiotaforhealth.com. Neuroscientist John Cryan warns that ignoring gut microbes is perilous: our immune system is “completely shaped by microbial signals,” and gut inflammation can “affect our mood and cause symptoms… similar to depression and anxiety” brainfacts.org.
Gut–Brain Axis: How Gut Bacteria Communicate with the Brain
The gut microbiota and brain are linked by the gut–brain axis – a bidirectional communication system. Gut microbes influence the brain via multiple pathways nature.com. For example, bacteria in the gut can produce neurotransmitters and metabolites (like short-chain fatty acids) that cross into the bloodstream or activate the vagus nerve, modulating brain function nature.com. Immune signals and hormones (e.g. cytokines, cortisol) released by gut tissues also reach the brain pmc.ncbi.nlm.nih.gov. In short, an intact gut is tied to normal brain function; as one review notes, “healthy gut function has been linked to normal CNS function” via hormones and neural signals pmc.ncbi.nlm.nih.gov. The gut even has its own nervous system (the ENS) with ~100 million neurons, earning it the nickname “second brain.” Recent research increasingly supports this view: a 2025 Scientific Reports collection emphasizes that vagal signaling from the gut regulates higher cognition (anxiety, depression, learning and memory) nature.com.
Impact on Mental Health: Depression, Anxiety and Stress
Human studies
Numerous studies have found altered gut microbiomes in mood disorders. For instance, a large Spanish cohort (n=400) found that participants with depression showed significant differences in gut bacteria composition and fecal metabolites compared to controls nature.com. Similarly, review articles report that gut dysbiosis and inflammation are linked to anxiety and depression pmc.ncbi.nlm.nih.gov. Harvard researchers note that the gut–brain link means gut distress can be both cause and effect of anxiety, stress or depression health.harvard.edu. Some small clinical trials hint at benefits from gut-targeted therapies: probiotic supplements have reduced anxiety/depression scores in some patients, suggesting rebalancing the microbiome may help mental health pmc.ncbi.nlm.nih.gov.
Animal studies
Animal experiments provide causal evidence. Germ-free rodents (raised without gut microbes) display exaggerated stress and anxiety-like responses brainfacts.org. In one landmark experiment, giving mice gut microbes from depressed people caused the animals to exhibit depressed, anxious behavior brainfacts.org. Conversely, researchers recently showed that transplanting microbiota from “stress-resilient” mice into stressed mice restored hippocampal neurogenesis and normalized their behavior pubmed.ncbi.nlm.nih.gov. These findings underline that specific bacterial communities can drive or alleviate depression/anxiety in animal models, though translating this to humans is an ongoing challenge.
Link to Cognitive Abilities: Memory, Learning and IQ
Human studies
Emerging human research links the gut microbiome to cognition. In a 2022 study of healthy young adults, those whose gut was dominated by Ruminococcaceae and Coriobacteriaceae bacteria scored higher on fluid intelligence (IQ) tests gutpathogens.biomedcentral.com. A broader review in Nutrients (2020) summarized 17 trials: nearly all probiotic/diet interventions saw improvements in cognitive tasks (spatial memory, verbal learning, attention) after manipulating the gut microbiome pubmed.ncbi.nlm.nih.gov. Pediatric studies also hint at connections: one study found school-age children with higher full-scale IQ tended to have more diverse gut flora, enriched in genera like Prevotella and Dialister frontiersin.org. Overall, higher microbiome diversity and specific bacterial taxa often correlate with better memory and reasoning, although causality is not yet proven.
Animal studies
Lab studies in animals show gut microbes can affect learning and memory. For example, mouse studies have demonstrated that altering the gut microbiota (via antibiotics or probiotics) can change performance on maze and memory tests. (Notably, germ-free mice often show deficits in learning and stress coping brainfacts.org.) Some studies report that specific bacterial strains improve rodent cognitive performance and brain plasticity markers. While animal cognition research is less extensive than mood studies, the consensus is growing that a healthy gut can support learning and memory in rodents, hinting at similar effects in humans.
Emerging Research and Theories
The field is rapidly evolving. Scientists are using multi-omics and large cohorts to map the gut–brain link. A 2025 analysis of hundreds of gut microbes found unique microbial “signatures” in depressed individuals, suggesting the gut may even influence neurotransmitter pathways in depression nature.com. The “second brain” concept (gut as an independent neural network) is gaining acceptance gutmicrobiotaforhealth.com, nature.com. For example, one theory posits gut microbes co-evolved with our nervous system, encoding primitive signals; today microbes respond to our neurotransmitters and in turn produce metabolites that feed back to brain cells. Some researchers have dubbed this field “psychobiotics,” exploring beneficial bacteria as mood and cognition treatments. However, many experts caution current data are preliminary: most human studies are small or correlative, and more trials are needed to prove cause-and-effect.
Diet, Probiotics and Gut-Health Interventions
The gut microbiome is highly modifiable by diet and supplements. High-fiber, plant-rich diets generally foster diverse, health-promoting microbes, while Western diets (high fat/sugar, low fiber) can disrupt the gut barrier and trigger inflammation isappscience.org. In experimental animals, a fiber-poor diet impairs the gut lining and allows microbial toxins to reach the bloodstream, which can ultimately affect the brain. Probiotic supplements (live beneficial bacteria) and prebiotics (foods that feed good bacteria) have shown promise in improving brain-related outcomes. For example, several controlled trials report that daily probiotics reduce anxiety, lower stress hormones, and in some cases enhance memory performance, likely by rebalancing gut flora pmc.ncbi.nlm.nih.gov. While no “magic pill” exists yet, maintaining gut health through diet (e.g. Mediterranean or plant-based diets) and targeted microbiome therapies is a leading idea for future cognitive and mental health care.
Sources: Scientific reviews and studies on the microbiome–brain axis pmc.ncbi.nlm.nih.gov, nature.com, gutpathogens.biomedcentral.com, pubmed.ncbi.nlm.nih.gov, plus expert interviews and institutional articles gutmicrobiotaforhealth.com, brainfacts.org, health.harvard.edu. These cover human and animal research findings, from cognitive tests to behavioral trials, and expert commentary on emerging gut-brain science.